Normwerte Nervenultraschall
Introduction
High-resolution ultrasound has emerged as a promising tool for scrutinizing peripheral neuropathies. In addition to many other features, it allows measurement of the cross-sectional area (CSA) of many peripheral nerves. Mainly, pathologies of the peripheral nervous system typically result in an enlargement of the nerve, which leads to an increase of the cross-sectional area (CSA). Conditions that cause such an enlargement often include entrapment neuropathies, and, less commonly, hereditary or acquired neuropathies, trauma, neural tumors, and others.
Many reports of nerve-CSA values have been published within the last decade and this topic is still evolving. However, reference values are still lacking for some nerves and those that have been published tend to show variability, probably due to factors such as measurement accuracy, expertise of the examiner, equipment, location of the nerve, and patient-specific factors (e.g., age or gender).
It should be noted that we are still not at the end of the journey and data that can correlate the CSA with ethnicity, age, gender, body mass, or height are still missing, but may significantly influence reference values. This means that we must be critical when using such measurements. We always need to correlate our findings with the clinical history/examination of the patient, and, if possible, with well-established methods (e.g., electro diagnostic tests) to confirm the diagnosis of a peripheral neuropathy.
What was our motivation
You are reading this article because you have the same passion as we, the authors. You like ultrasound. You perform it to diagnose peripheral neuropathies. At least five times, you’ve asked your teacher, supervisor, or colleague about CSA reference values. Moreover, at least some of you have searched for data in books or publications to become familiar with nerve reference values. Don´t worry: we also have the same problem and are still searching the literature to obtain information about correct values. This was our motivation! We wanted to summarize information about nerve CSA and to generate some tool that might immediately help you in daily clinical routine. In our opinion, a Pocket Card is a good choice because you can take it wherever you want and it fits into most of our hospital coats. Besides some limitations that are mentioned in the limitation section, we think we created a good basic pocket card, which will surely need adaptations in the future.
How we did it
We searched the literature in pubmed and google scholar for cross-sectional area and nerve. It was not the aim of this Pocket Card to be statistically absolutely correct. We collected publications where at least mean and standard deviations were provided. We then checked the publications for correct measurements of the CSA (please see below), to determine whether at least some words about data collection and measurements and ultrasound images were provided. Further, we summarized all mean- and SD-values and built a reference value, as you can see on the pocket card.
What are the limitations
Statistically, the summation of the mean and SD does not represent an absolutely correct method with which to summarize data from studies with different methods. Nevertheless, we think the CSA reference values as presented here are a good possibility to start with, because the mean values did not show high differences or outliers when compared.
No correlation was performed with parameters such as age, ethnicity, gender, body mass, or height. We think these parameters may have an influence on CSA, which was already shown in some small studies, and need to be considered in the future when sufficient data is available to underline this. If you are an interested reader of publications concerning CSA and nerves, you probably will miss some studies. The reason is simple. We excluded studies which did not provide mean and SD values or where we could not identify ultrasound images and/or reproducible measurements.
How to perform the examination
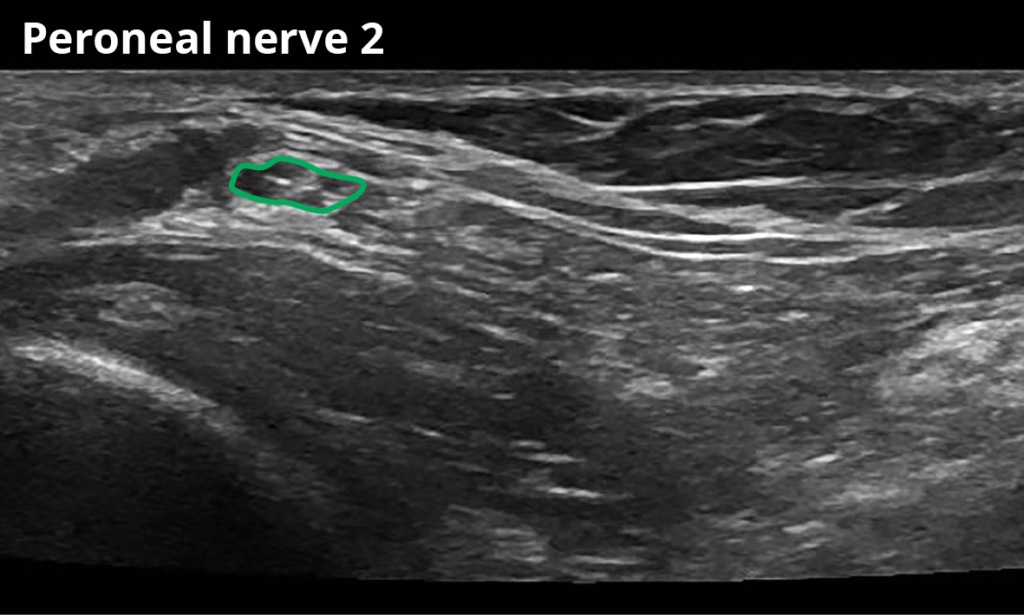
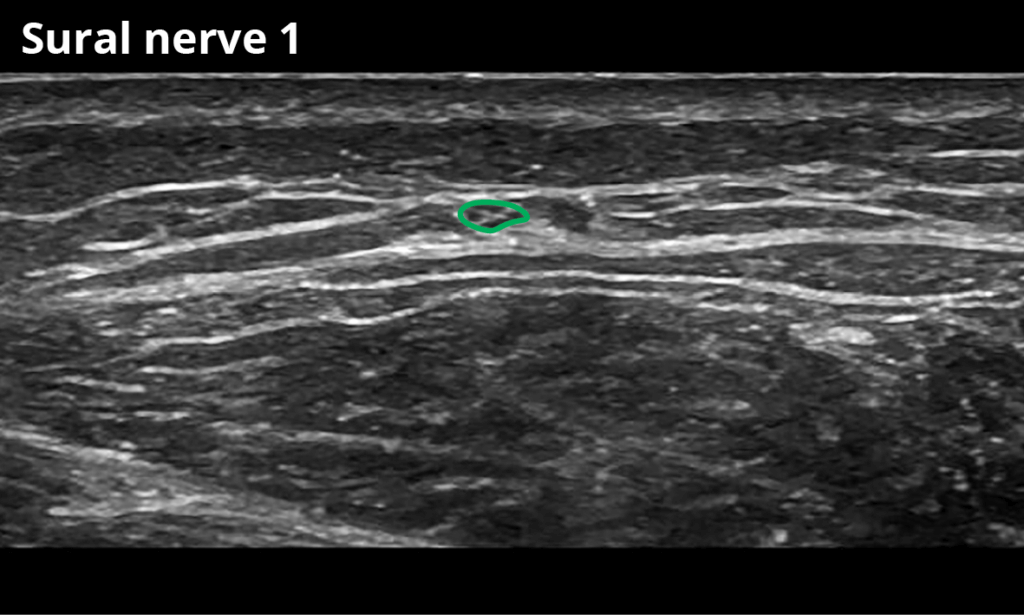
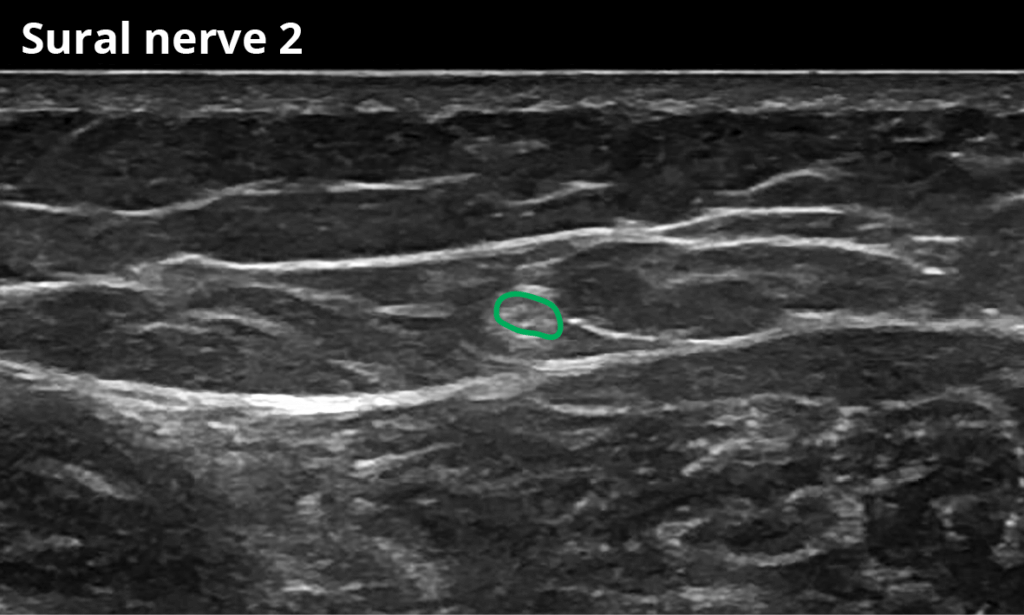
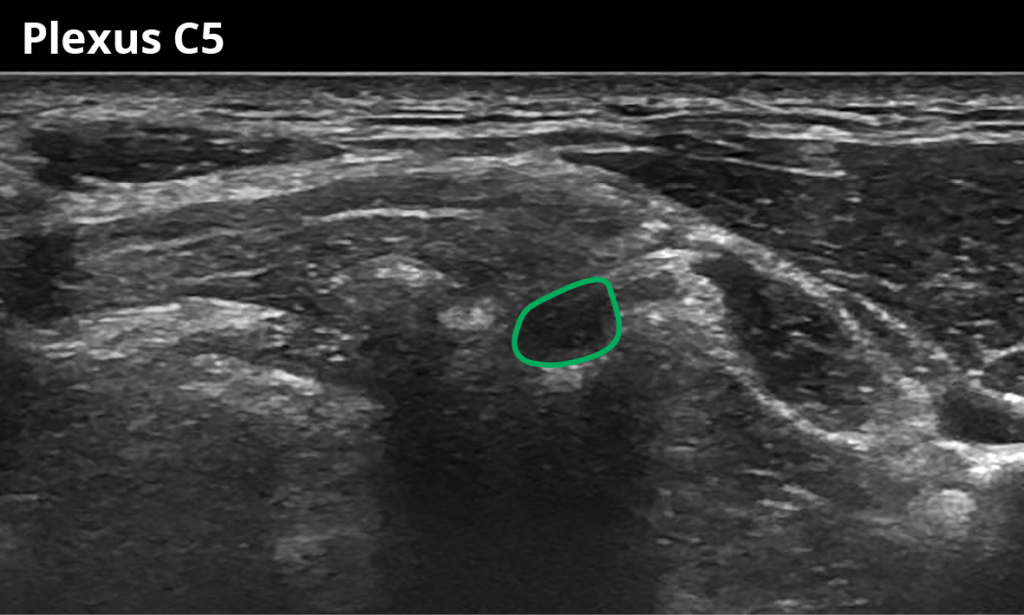
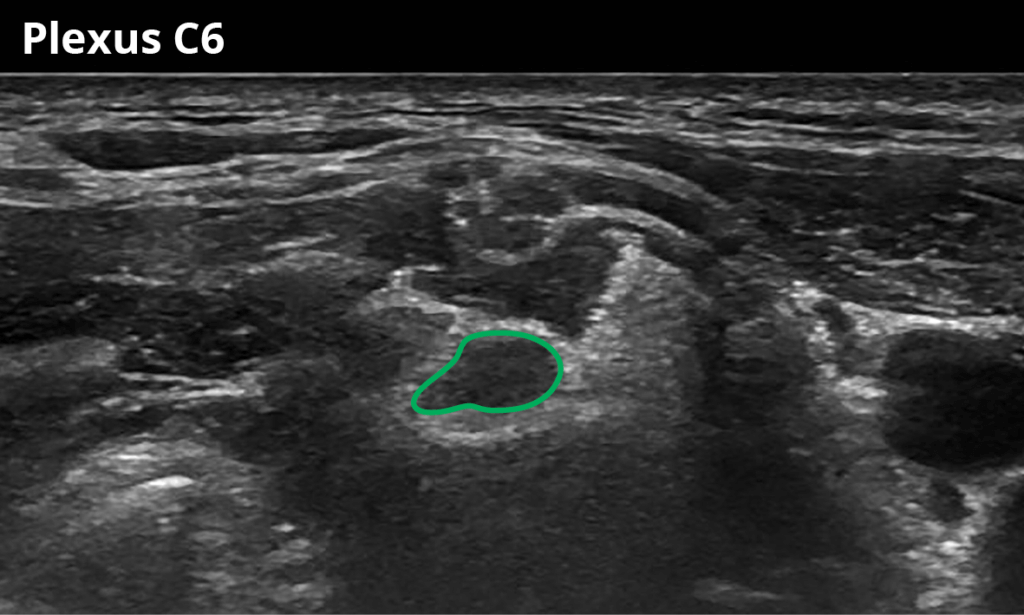
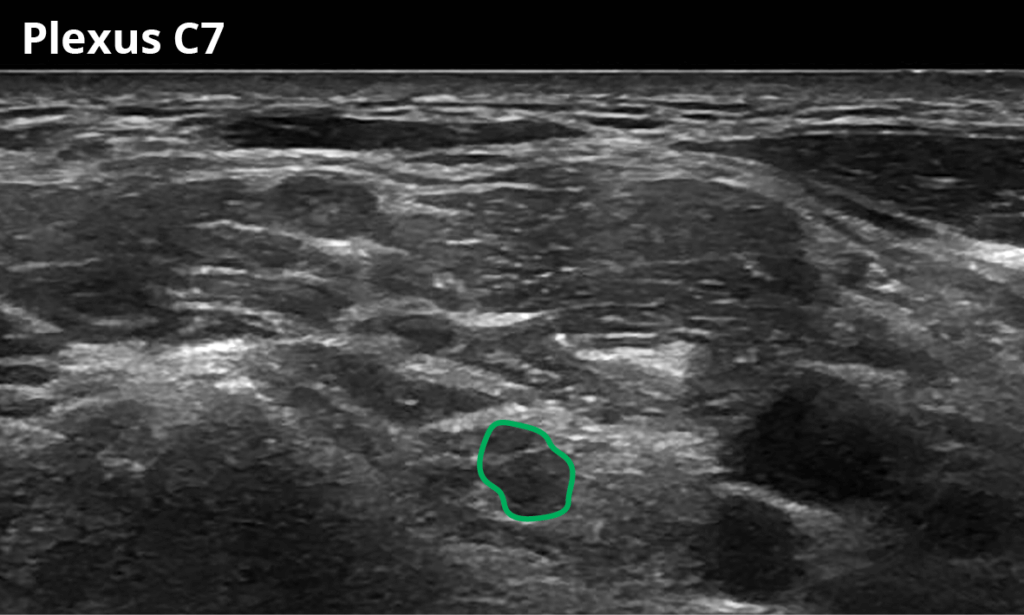
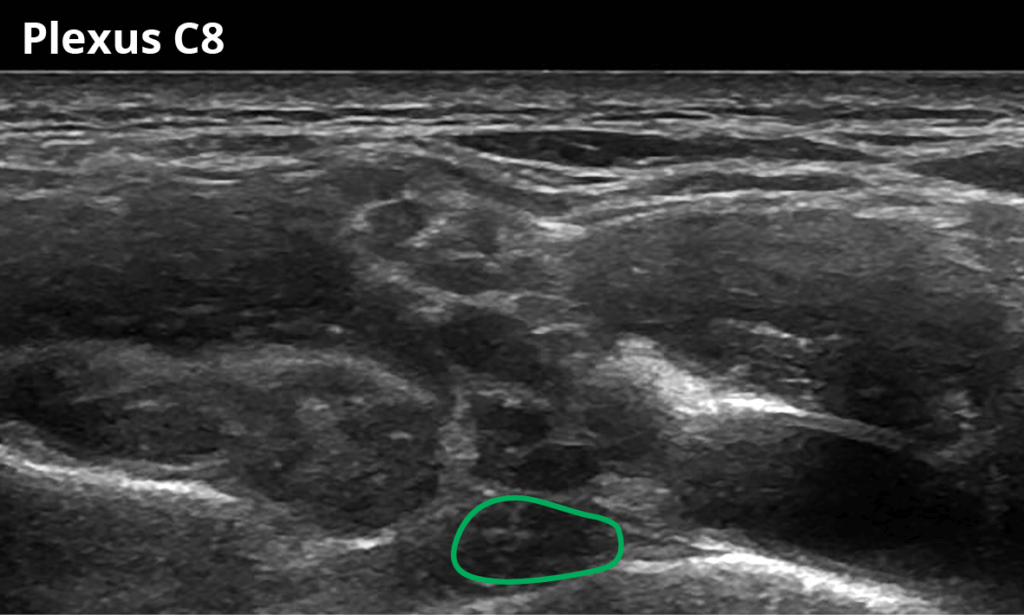
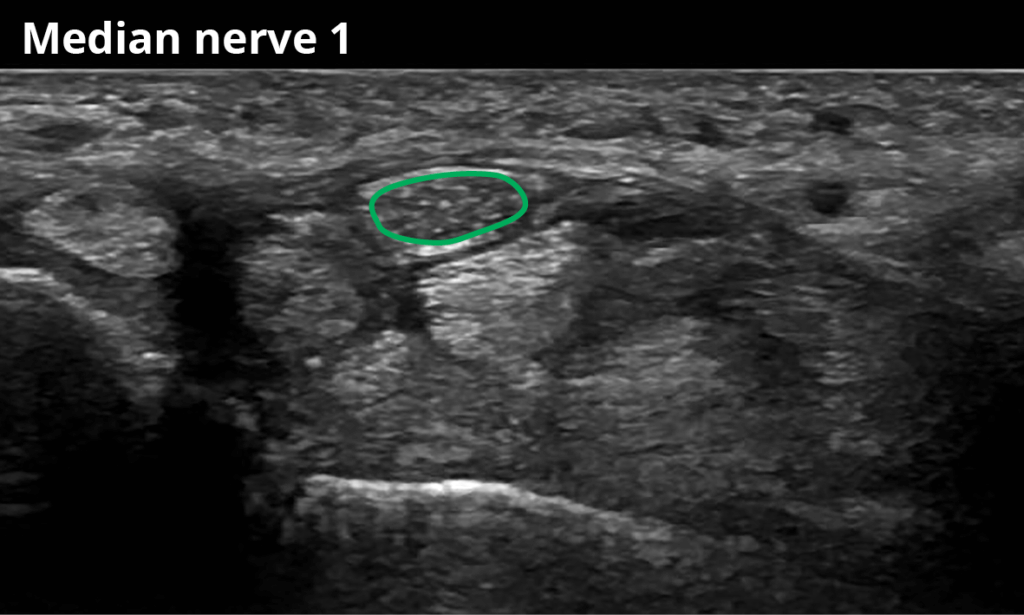
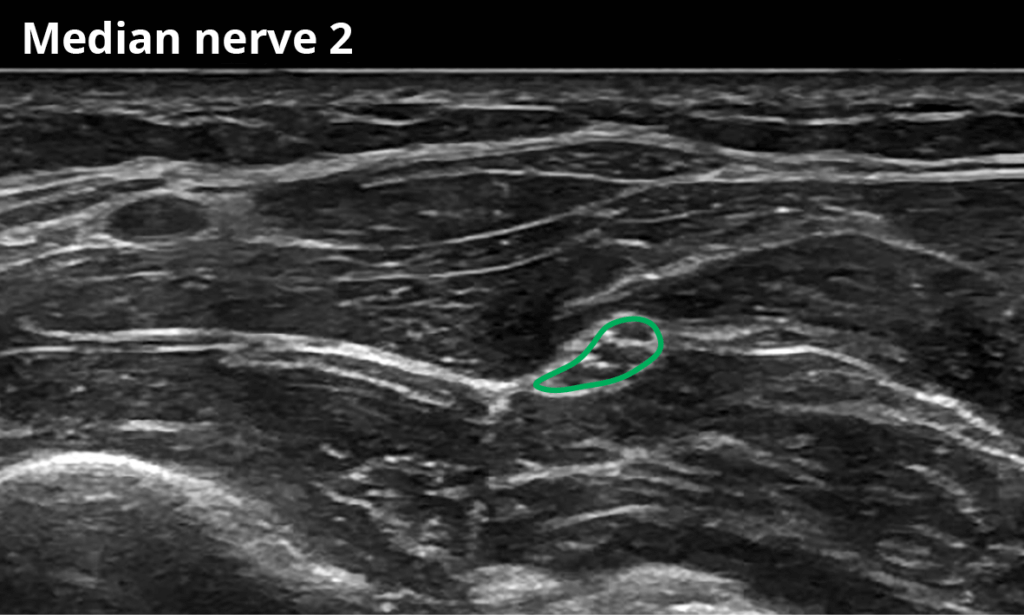
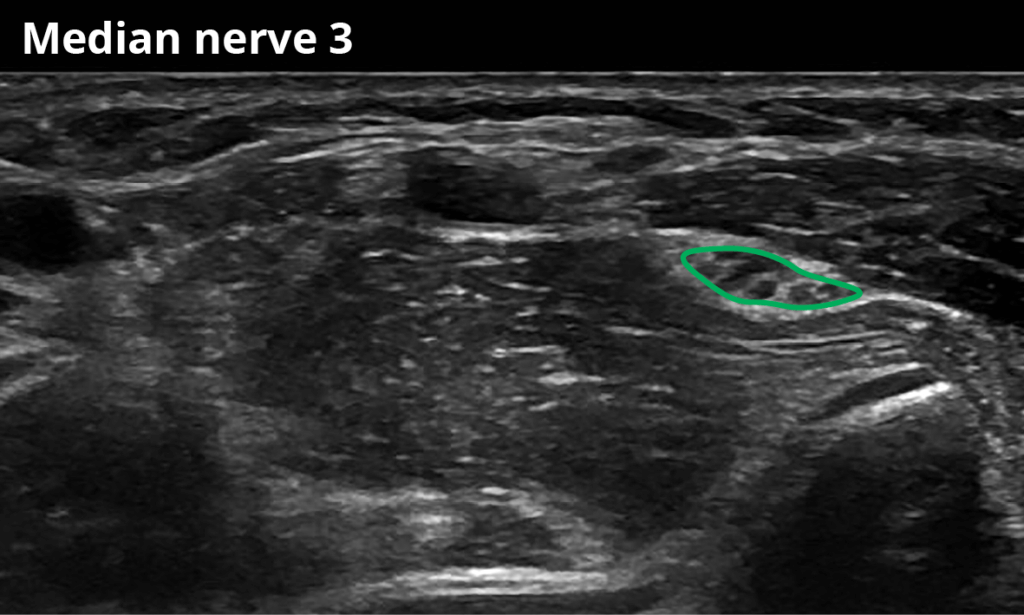
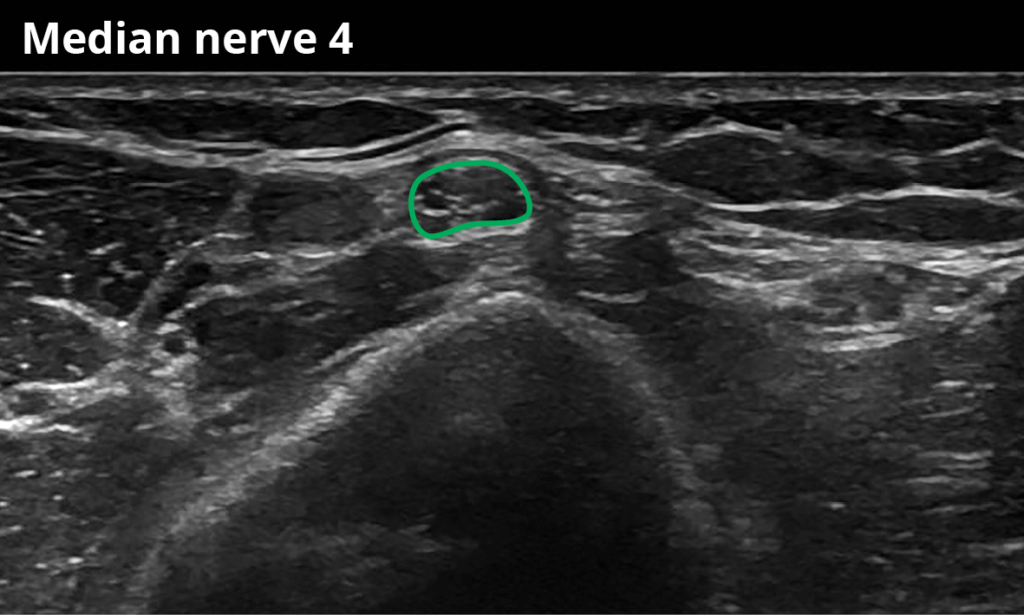
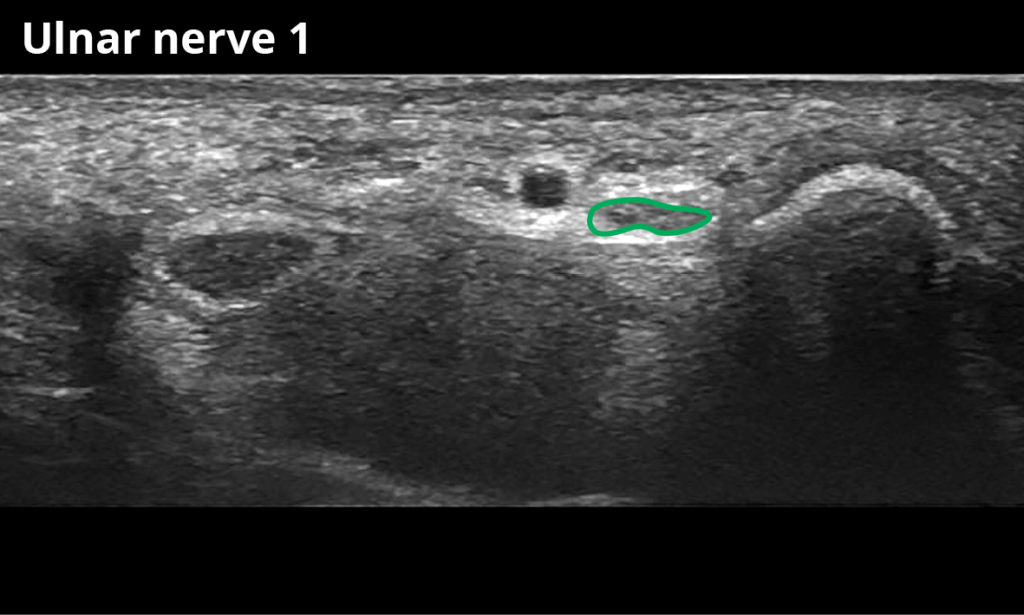
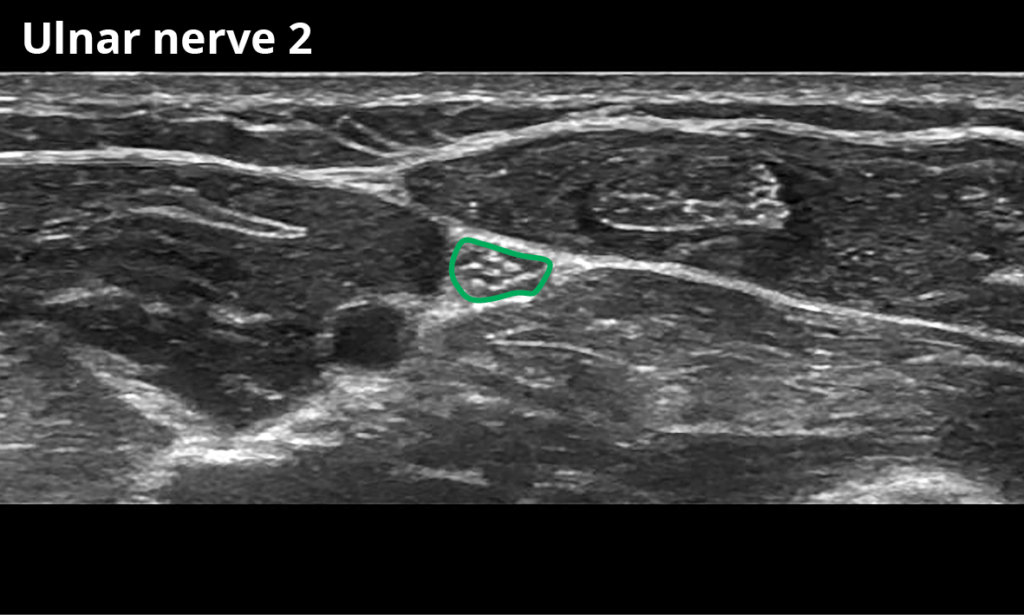
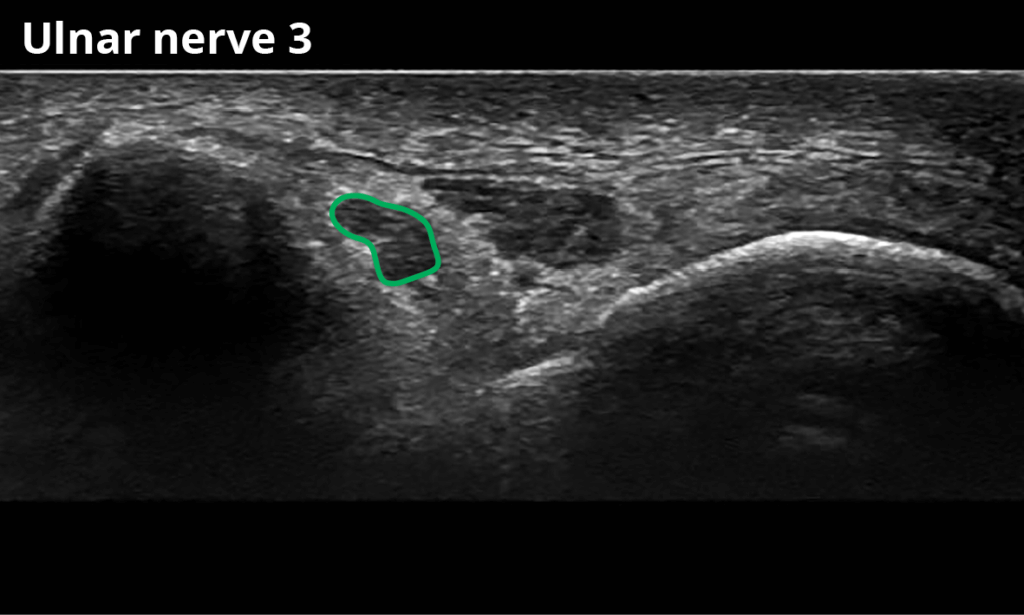
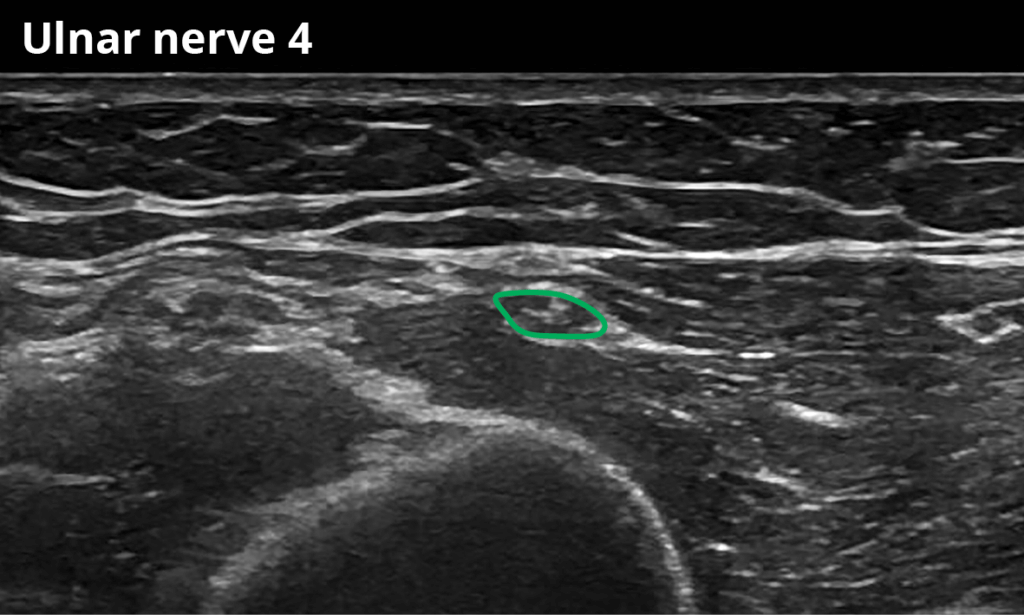
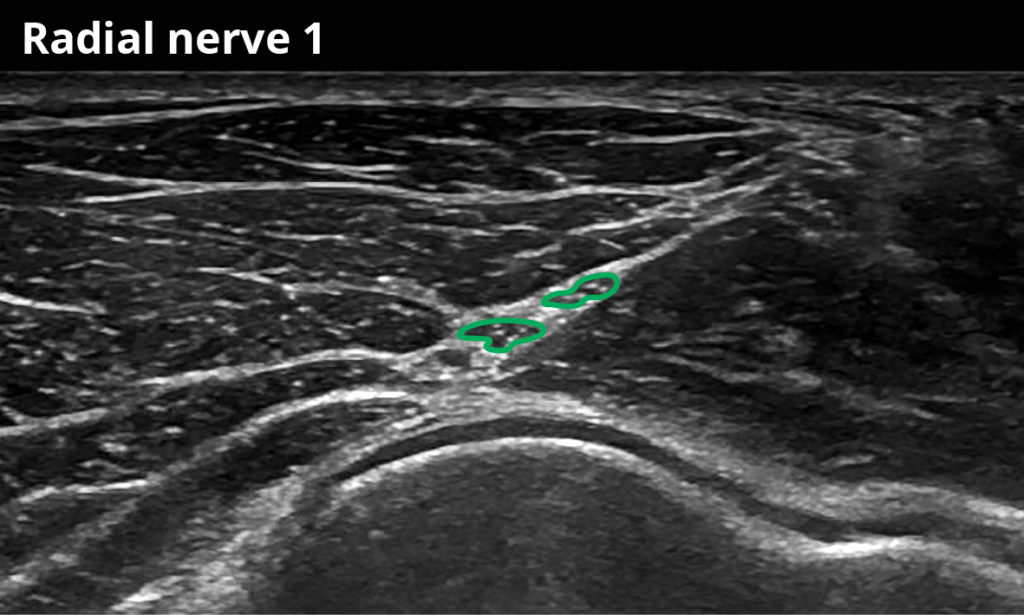
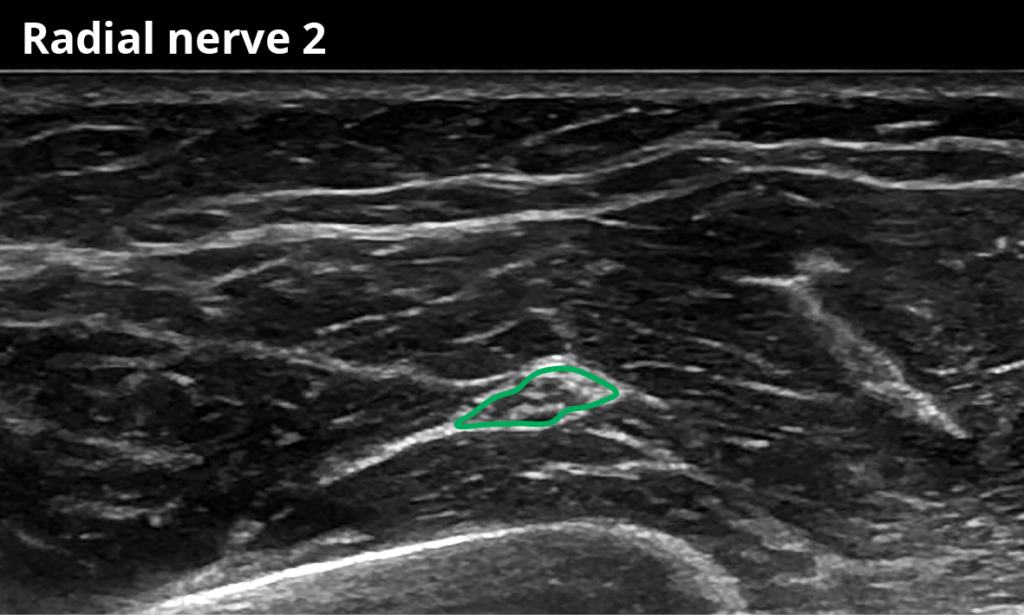
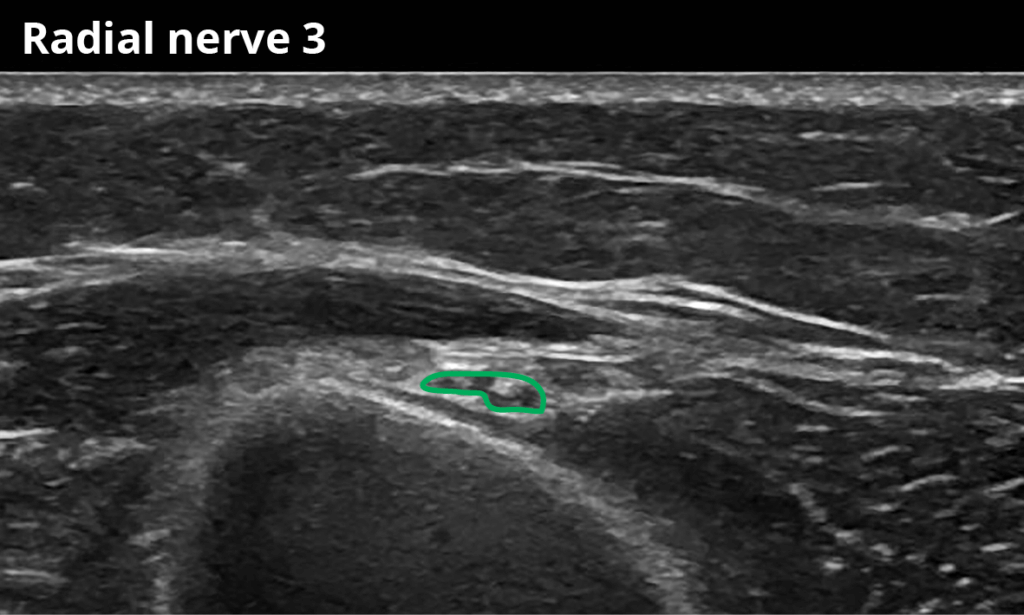
The CSA of the nerves needs to be measured using the trace function of the ultrasound device by manually tracing inside the hyperechoic rim of each nerve. The angle of insonation needs to be adjusted perpendicular to the nerve to avoid anisotropy and incorrect measurements. In this position, the nerve appears the brightest with the best discernible outer margins.
To facilitate CSA-measurements and to correctly identify the location of the nerves, we have provided images of the nerves at different locations. Please see the figures below.
We hope you enjoy our Pocket Card and we hope it helps you in daily clinical routine. We want to spread this knowledge, so please tell your colleagues all over the world that such a thing exists and how they may find it.
Acknowledgment
Many friends helped us to provide this Pocket Card. We want to thank the students of the Medical University Vienna who helped with the literature search and to obtain good ultrasound images. Further, we want to thank Mary Mc Allister who proofread the English version of this description. Last but not least, the man behind the illustrations is Aron Cserveny (sciencevisual.at) who has supported us for some years and took all of our work to another level.
Important note:
Measuring the CSA is only a small part of nerve imaging and can never be the only part of such an examination. It is an adjunct to further confirm your findings and nothing more. To diagnose neuropathies with ultrasound you need special ultrasound knowledge about the musculoskeletal system and other structures surrounding the nerves (e.g., vessels). Always keep in mind: Your diagnosis immediately influences a patient’s further treatment. An incorrect diagnosis may harm the patient. If in doubt, seek advice from an expert and never stop gaining ultrasound knowledge, either by examining many patients, taking courses, or reading the newest publications.
Figures
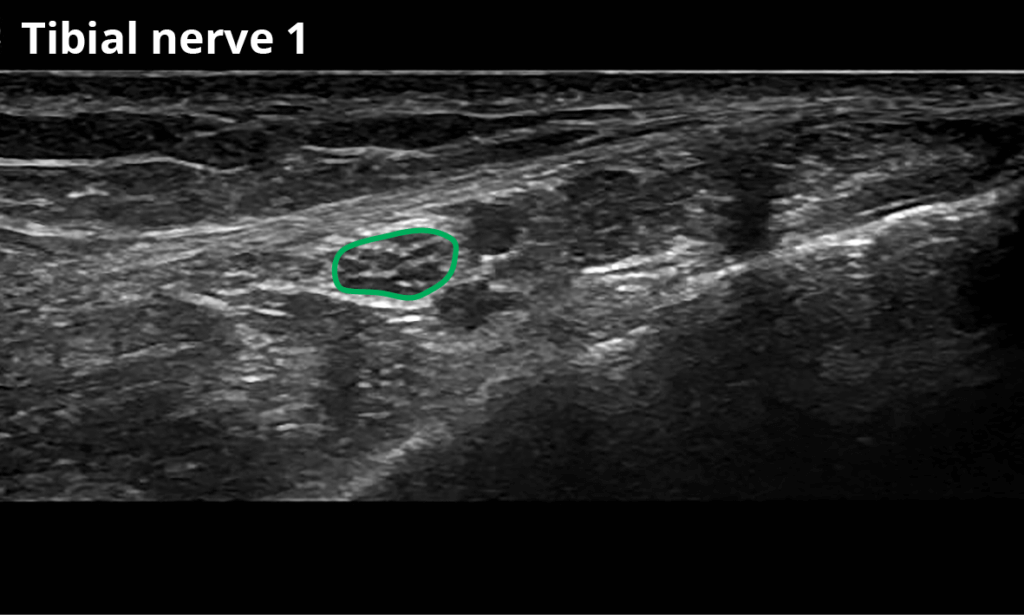
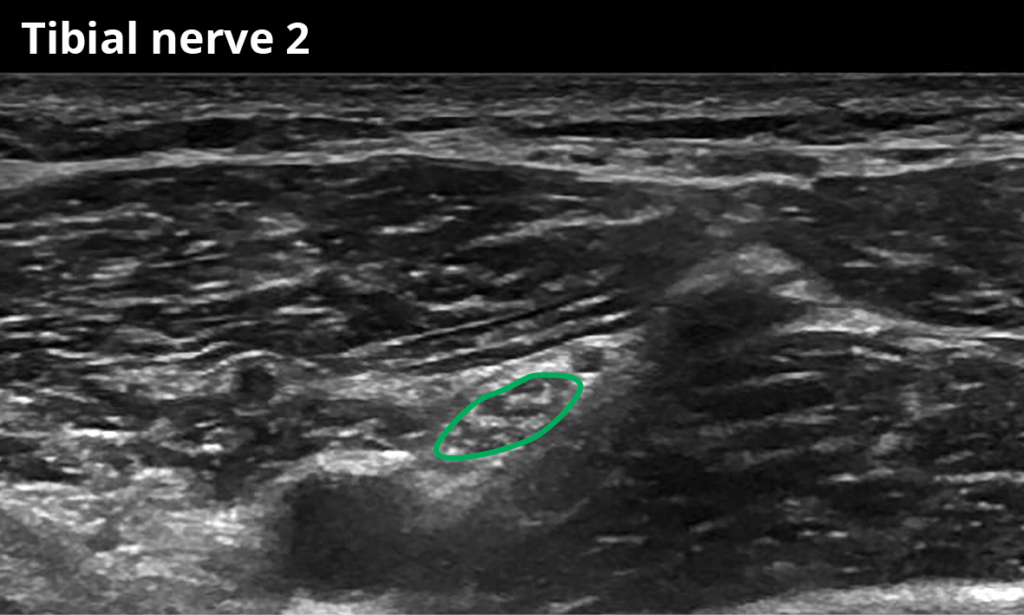
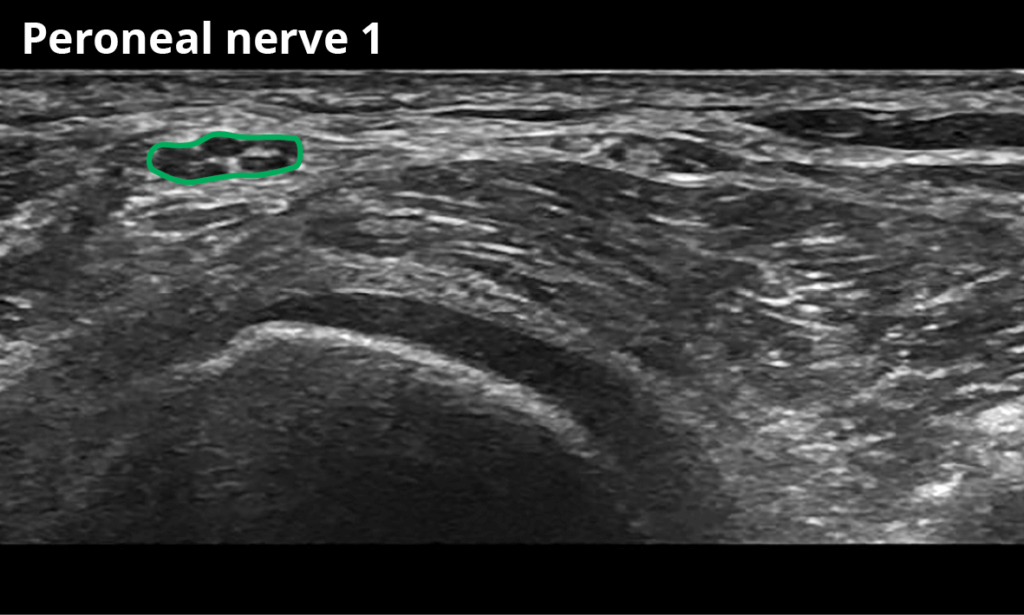
The subjects are supine during ultrasonography of the median, ulnar, radial nerve, and the brachial plexus, and prone when examining the tibial, fibular, and sural nerves.
Tibial nerve:
1 At the ankle within the posterior tibial tunnel (10,7 ± 3,4 mm²)
2 Within the popliteal fossa, distal to the bifurcation of the sciatic nerve (18,0 ± 6,4 mm²)
Peroneal nerve:
1 Below the fibular head (9,5 ± 2,8 mm²)
2 Within the popliteal fossa, distal to the bifurcation of the sciatic nerve (10,2 ± 3,6 mm²)
Sural nerve:
1 In the distal calf just proximal to the lateral malleolus (4,0 ± 1,5 mm²)
2 Between the lateral and medial head of the gastrocnemius muscle (approximately 20 cm proximal to the medial malleolus) (1,8 ± 0,6 mm²)
Plexus (all roots):
1 Just after the nerve root exits over the transverse process of C5 (6,4 ± 1,8 mm²)
2 Just after the nerve root exits over the transverse process of C6 (8,6 ± 2,4 mm²)
3 Just after the nerve root exits over the transverse process of C7 (11,1 ± 2,6 mm²)
4 Just after the nerve root exits over the transverse process of C8 (10,7 ± 2,4 mm²)
Median nerve:
1 At the entrance of the carpal tunnel (thickest nerve cross-sectional area) (9,2 ± 2,1 mm²)
2 At the mid-forearm between the deep and superficial flexor muscles ( 7,2 ± 1,6 mm²)
3 At the elbow next to the brachial artery (9,2 ± 2,4 mm²)
4 Within the mid-proximal upper arm ( 9,2 ± 2,1 mm²)
Ulnar nerve:
1 At the level of the pisiform bone (Loge de Guyon) (4,9 ± 1,0 mm²)
2 At the mid-forearm (5,6 ± 1,0 mm²)
3 In the Sulcus between the medial epicondyle and olecranon (6,3 ± 1,4 mm²)
4 At the mid-upper arm (5,9 ± 1,2 mm²)
Radial nerve:
1s Approximately 1cm distal of the radial nerve bifurcation (superficial branch: 2,1 ± 0,6mm²)
1p Approximately 1cm distal of the radial nerve bifurcation (deep branch: 2,0 ± 0,4 mm²)
2 At the antecubital fossa just proximal to the radial nerve bifurcation (4,5 ± 0,7 mm²)
3 At the spiral groove (4,6 ± 1,3 mm²)
Literature
1. Bathala L, Kumar P, Kumar K, Visser LH. Ultrasonographic cross-sectional area normal values of the ulnar nerve along its course in the arm with electrophysiological correlations in 100 Asian subjects. Muscle & nerve. 2013 May;47(5):673-6.
2. Bedewi MA, Abodonya A, Kotb M, et al. Estimation of ultrasound reference values for the lower limb peripheral nerves in adults: A cross-sectional study. Medicine. 2018 Mar;97(12):e0179.
3. Bedewi MA, Yousef AM, Abd-Elghany AA, El-Sharkawy MS, Awad EM. Estimation of ultrasound reference values for the ulnar nerve fascicular number and cross-sectional area in young males: A cross-sectional study. Medicine. 2017 Mar;96(10):e6204.
4. Boehm J, Scheidl E, Bereczki D, Schelle T, Aranyi Z. High-resolution ultrasonography of peripheral nerves: measurements on 14 nerve segments in 56 healthy subjects and reliability assessments. Ultraschall in der Medizin. 2014 Oct;35(5):459-67.
5. Cartwright MS, Passmore LV, Yoon JS, Brown ME, Caress JB, Walker FO. Cross-sectional area reference values for nerve ultrasonography. Muscle & nerve. 2008 May;37(5):566-71.
6. Cartwright MS, Shin HW, Passmore LV, Walker FO. Ultrasonographic findings of the normal ulnar nerve in adults. Archives of physical medicine and rehabilitation. 2007 Mar;88(3):394-6.
7. Chang KV, Wu WT, Han DS, Ozcakar L. Ulnar Nerve Cross-Sectional Area for the Diagnosis of Cubital Tunnel Syndrome: A Meta-Analysis of Ultrasonographic Measurements. Archives of physical medicine and rehabilitation. 2018 Apr;99(4):743-57.
8. Hobson-Webb LD, Massey JM, Juel VC, Sanders DB. The ultrasonographic wrist-to-forearm median nerve area ratio in carpal tunnel syndrome. Clinical neurophysiology : official journal of the International Federation of Clinical Neurophysiology. 2008 Jun;119(6):1353-7.
9. Kerasnoudis A, Pitarokoili K, Behrendt V, Gold R, Yoon MS. Cross sectional area reference values for sonography of peripheral nerves and brachial plexus. Clinical neurophysiology : official journal of the International Federation of Clinical Neurophysiology. 2013 Sep;124(9):1881-8.
10. Kim JH, Won SJ, Rhee WI, Park HJ, Hong HM. Diagnostic cutoff value for ultrasonography in the ulnar neuropathy at the elbow. Annals of rehabilitation medicine. 2015 Apr;39(2):170-5.
11. Kim JY, Song S, Park HJ, Rhee WI, Won SJ. Diagnostic Cutoff Value for Ultrasonography of the Common Fibular Neuropathy at the Fibular Head. Annals of rehabilitation medicine. 2016 Dec;40(6):1057-63.
12. Qrimli M, Ebadi H, Breiner A, et al. Reference values for ultrasonograpy of peripheral nerves. Muscle & nerve. 2016 Apr;53(4):538-44.
13. Tagliafico A, Cadoni A, Fisci E, Bignotti B, Padua L, Martinoli C. Reliability of side-to-side ultrasound cross-sectional area measurements of lower extremity nerves in healthy subjects. Muscle & nerve. 2012 Nov;46(5):717-22.
14. Won SJ, Kim BJ, Park KS, Yoon JS, Choi H. Reference values for nerve ultrasonography in the upper extremity. Muscle & nerve. 2013 Jun;47(6):864-71.
15. Yalcin E, Onder B, Akyuz M. Ulnar nerve measurements in healthy individuals to obtain reference values. Rheumatol Int. 2013 May;33(5):1143-7.